Understanding Shoulder Pain
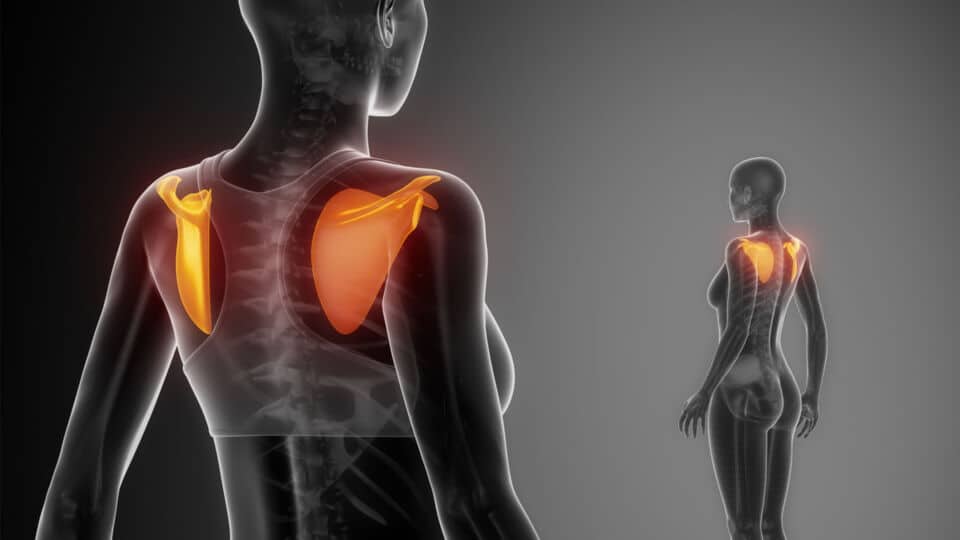
The shoulder joint is the most mobile joint in the body. With all these motion, it is little wonder that the shoulder is a common cause of pain.
There are many causes of shoulder pain and most of these can be diagnosed through a good history and clinical examination. Some of the common causes are:
• Tendinitis
• Rotator Cuff tear
• Frozen Shoulder
• SLAP
• Arthritis of the acromioclavicular and glenohumeral joint
Rotator Cuff Tendinitis
Rotator cuff tendinitis is a very common cause of pain in the shoulder. It is much more common source of pain than frozen shoulder. Patients typically complain of pain with certain movements. At times they describe it as “catching sensation”.
They may complain of pain when they take off their T shirts, buckling their inner garment for women, or reaching behind for their wallets or tucking in their shirt for men.
The mechanism of injury is often due to over extension. Very often it is a driver of a car trying to reach in the back seat for an object that develops this. It may also be a tennis player doing an overhead serve without turning his or her trunk resulting in an over extension of the shoulder.
Some individuals are prone to developing this because of external impingement from a bone spur or a non compliance coracoacromial (CA) ligament.
The rotator cuff tendon is housed in the subacromial space; the floor is the greater tuberosity and the roof is an osseous-fibrous roof consisting of the CA ligament in front and the acromion behind (Fig 1).
The tendon can sometimes be “squeezed” or pinched by the bony “floor” and bony “roof”, especially if there is a sharp bone spur at the acromion or a non compliance CA ligament. Others may have a congenitally hook acromion or os acromiale which may cause the impingement.
A supraspinatous outlet view is useful to visualize this spur. An axillary view is also needed to exclude any os acromiale syndrome.
The treatment is usually a course of NASIDs or a hydrocortisone and lignocaine (H&L) injection to the subacromial space. However, if a complete tear is suspected, an H&L should not be performed. Patients who display weakness after the H&L or does not respond to the H&L should have a MRI of the shoulder to exclude any tear in the rotator cuff muscle.
Rotator Cuff Tear
Individuals may suffer from rotator cuff tear when they fall on an outstretched hand or collide with something or someone. Overhead sports like badminton, swimming, tennis, basketball, volleyball, rock climbing and weight lifting can also result in repetitive injury to the rotator cuff.
Many a time it may also be due to recurrent tendinitis leading to an attrition tear (Fig 2). So there may not be a definitive event that a patient can recall.
Very often a person suffering from rotator cuff tear may have a bone spur predisposing that individual to a tear (Fig 3).
Aside from symptoms of tendinitis, one may also experience weakness in the shoulder. They have weakness or pain on elevation or abduction. However, these patients have full passive range of motion. This clearly distinguishes them from frozen shoulder where both active and passive range of motion is equally restricted.
In the natural history of a cuff tear, the condition will progress and may lead to cuff tear arthropathy in 5 to 10 years. Thus patients with rotator cuff tear are recommended to undergo arthroscopic rotator cuff repair and acromioplasty (removal of the spur). This is carried out with three to four small stab incisions of 0.5cm in length around the shoulder.
Frozen Shoulder
Frozen shoulder, or adhesive capsulitis, is a condition that creates pain and stiffness in the shoulder. The stiffness is usually global, i.e. the shoulder is restricted in all directions. Patients have difficulty raising their arm in front of them, from the side, behind their back and behind their head.
This is a problem with the capsule of the shoulder joint. This capsule may thicken and the ligaments shorten due to inflammation. As a result of this, mobility is greatly reduced in the shoulder.
Frozen shoulder can happen after a shoulder injury or after knocking the shoulder against something or someone. Very often it develops in individuals above 40 years with no apparent reason. It is also more likely to appear in women. Diabetes, heart disease, lung disease, thyroid, stroke or rheumatoid arthritis also put one at higher risk of developing this.
This condition is different from rotator cuff tear in that its passive range of motion is also restricted to the same degree as the active. The treatment algorithm is usually a trial of conservative treatment.
One can try physiotherapy for 6 weeks; if there is little improvement, then a cortisone injection into the gleno-humeral joint is recommended. It is a myth that all cases of frozen shoulder can be treated conservatively.
Recent literatures have suggested that at least 10 to 50 % of frozen shoulder still has residual stiffness and limited range of motion after 5 years. If the condition shows little improvement after 6 months of diligent physiotherapy, patient should be offered an arthroscopic capsular release (ACR).
Manipulation under anesthesia comes with risks of humeral fracture and rotator cuff tear; hence it is discouraged.
Arthroscopic capsular release, on the other hand, allows controlled release of the capsule and has significantly fewer complications.
SLAP
SLAP stands for Superior Labral from Anterior to Posterior tear. It is a tear of the labrum in the glenohumeral joint from the 3 o’clock to the 9 o’clock position (Fig 3). The patient often complains of pain with overhead activities together with rotation of the arm.
There is often a clicking sound associated with it. The mechanism of the injury is often from a fall on an outstretched hand, traction injury to the shoulder or repetitive overhead sports. In the local context, many patients actually develop this kind of tear from the pull up bars.
During dismount one hand may still be hanging from the bar and they may sustain traction and twisting force to the shoulder.
Clinical tests for SLAP include the crank test and O’Brien stress test. They may also have pain with the arm abducted at 90 degrees and externally rotated.
Xrays usually show normal findings in these individuals. MRI alone may miss a SLAP tear, so MR arthrogram is the choice of investigation.
Most SLAP tears can be treated conservatively but a small number of cases may require an arthroscopic repair of the biceps and labrum.
Arthritis of the Acromioclavicular and Glenohumeral Joint
Arthritis can be due to many factors. It may be a result of frequent dislocation, post injury, rheumatoid, primary osteoarthritis or chronic rotator cuff tear. It may involve the glenohumeral joint (Fig 4) or the acromioclavicular joint (Fig 5).
Patients often complain of a dull pain in the shoulder. They will have early morning stiffness that gets better as the day gets on but only becomes painful again at night. If severe, this may affect one’s sleep or may even persist throughout the day. They will have difficulty and pain lying on the affected shoulder at night.
In acromioclavicular joint arthritis, there may be pain on the top of the shoulder. There is pain when reaching to touch the other shoulder or above your head.
In rotator cuff tear arthropathy (chronic rotator cuff tear leading to arthritis of the glenohumeral joint), patients often have pain and pseudoparalysis of the shoulder. As they have rotator cuff tear, they are unable to lift the shoulder as if their shoulder is paralysed.
Over time the eccentric wear of the glenoid causes arthritis. These patients are best treated with a new shoulder replacement implant called reverse shoulder arthoplasty.
This implant is different from the traditional shoulder replacement as it reverses the configuration of the glenohumeral joint such that the glenoid now becomes a ball and the humeral head becomes a cup.
It increases the moment arm of the deltoid and hence allows for elevation of the shoulder after the replacement. As it replaces the articular surface of the shoulder, it relieves pain as well (Fig 6).
Conclusion
Each of the above pathology has a very distinct history and pattern of pain. However it is important to come to an accurate diagnosis so that your patient can be treated appropriately with the most up to date form of management for each of the problem.



