Female Fertility Tests
Assessment of female fertility begins firstly with a record of your menstrual dates. You should take notes of the first days of your recent menses so as to know the pattern of your menstrual cycles.
On top of these, you may need to take additional tests to ascertain your egg reserve and whether you ovulate or not.
- Female Fertility Test For Egg Reserves
- Female Fertility Test For Ovulation
- Female Fertility Test For Other Assessments
- Male Fertility Tests
- Other Fertility Tests and Treatments
If you have been trying to conceive naturally for a while with no success, the first step is to take a fertility test. Learn more about the Raffles Fertility Test for Couples.
Female Fertility Test For Egg Reserve
This is useful for women who are concerned about their store of eggs, especially for those who had blood cysts in their ovary, previous ovarian surgery and in women above 35 years old. Women whose mothers or sisters reached menopause before the age of 40 years should also get an assessment of their egg reserves.
Antral follicle count
The Antral Follicle count is conducted using transvaginal ultrasound scans. The fertility specialist will perform ultrasound scans in the clinic by inserting the ultrasound probe into the vagina. The procedure is safe and not painful.
The antral follicles appear as small dark shadows measuring between 2 to 8 mm in diameter. They represent the follicles which contain eggs. By simply counting of the number of antral follicles, we get a snapshot of your egg reserves and whether you have sufficient eggs.
Antral follicles represent only a cohort of immature eggs at a certain stage of development. Eggs that are not developed yet (primordial follicles) do not have visible follicles.
Eggs that develop beyond the antral follicles appear as larger follicles of various sizes, usually larger than 10mm. One of them will grow faster and larger becoming a dominant follicle, containing a maturing egg.
This dominant lead follicle will usually ovulate when it is between 16mm and 26mm in size. The other follicles in the same cohort will then shrink and disappear, while the eggs within will degenerate.
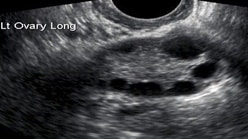

Transvaginal Ultrasound scans of the ovary showing antral follicles
AMH level
The Anti-Mullerian Hormone (AMH) level can be measured via a blood test. The Anti-Mullerian Hormone is secreted by granulosa cells of the antral follicles. The AMH level thus reflects the amount of antral follicles a woman has at a specific point of time.
The AMH level is a fairly accurate indicator of a woman’s ovarian or egg reserve. AMH test can be done any time during the menstrual cycle. It is often done in women before assisted reproduction programmes to assess the likely response to fertility medications and to adjust the dosage needed.
Some studies now show that AMH level may also be correlated to pregnancy chances although it cannot be used to predict success rates in fertility programmes.
Female Fertility Test For Ovulation
Urine LH test
The urine LH test is a self-administered test to identify when ovulation will occur. This test detects the LH (Luteinising Hormone) which rises sharply 24 to 36 hours before ovulation.
It may not be easy to detect the LH surge as it requires the test to be conducted on the right day and time. This means you may have to test over a few days before ovulation.
In women with ovulation problems, the baseline LH may be high causing false positive results. In women with irregular menses cycles, this method may not be useful as it is often difficult to determine which days to perform the test.
Ultrasound scans
These are useful for monitoring of the follicles (egg cysts) in the ovary and hence, to estimate when ovulation is likely to occur. Doing transvaginal ultrasound scans over several days of your menstrual cycle to monitor the growth of the follicles is called follicular tracking.
By measuring the diameter of the dominant follicle, believed to contain a mature egg, an estimation of the possible timing of ovulation can be made. If the follicles do not grow, there is no ovulation. If the menstrual cycle is irregular and delayed, more scans may be needed to track the follicular development.




Transvaginal Ultrasound scans of the ovary showing dominant follicle
Progesterone level about 7 days after ovulation or 7 days before expected date of next menses
Progesterone is produced by the ovary after ovulation. It has an important function to convert the endometrium (inner wall of uterus) to its secretory stage to prepare for implantation.
The level starts to increase after ovulation and reaches high levels after a few days. It remains high but reduces rapidly about 2-3 days before the next menses starts. Menses usually come 14 days after ovulation.
Doing a blood test of this hormone is useful to check whether ovulation has occurred. Unfortunately progesterone level varies during different times of the day. Only low or high levels are useful for interpretation. If the level of progesterone is low, ovulation has not occurred. If it is high, ovulation has occurred.
Female Fertility Tests For Other Assessments
Pelvic Assessment by Transvaginal Ultrasound scans
This is an essential test as it gives the fertility specialist an insight of the organs of the pelvis. Unlike the Transabdominal Ultrasound scans of the Pelvis when patient should have a full bladder to have better ultrasound images of the pelvis, Transvaginal scans are best done with the bladder empty for close up images of the pelvic organs and to assess the mobility of the pelvic organs. This is to detect any suspicion of the following conditions:
- Adenomyosis (enlargement of the uterus due to endometriosis of the uterus)
- Hydrosalpinges (swollen fallopian tubes)
- Uterine abnormalities - polyps, fibroids, double uterus, uterine septum
- Ovarian cysts - blood cysts, polycystic ovary, benign and malignant ovarian cysts
- Antral follicle count (an estimation of egg or ovarian reserves)
Hormonal Test to measure hormones that control the menstrual cycles
Menstruation is the cyclic shedding of the uterine lining, in response to the interactions of the hormones from hypothalamus and pituitary glands in the brain and the ovaries. The hormones controlling development of the eggs are FSH and LH from the pituitary gland. Their levels should be low at the beginning of the menstrual cycles and increases as the cycle progresses.
Hormones controlling other organs can affect ovulation, notably a raised TSH level due to hypothyroid condition. A high Prolactin level can also affect ovulation. Other hormone tests may also be performed if you have irregular menstrual cycles are:
| Basic Hormonal Profile | Additional Specialized Hormonal Tests (for specific situations as advised by your OBGYN) |
|---|---|
| Day 3 to 5 FSH level | TSH level |
| Day 3 to 5 LH level | PRL level |
| Day 3 to 5 E2 level | DHEAS level |
| Anti-Mullerian Hormone level | Testosterone level |
| Insulin level (fasting) |
Male Fertility Tests
Male fertility tests can begin with a simple sperm test. Make sure the test is done by a laboratory specialising in fertility. Results from the basic biochemical laboratory may not adhere to the strict WHO standards.
Semen analysis (also called a “sperm count’) is more accurate if performed on a sample collected after abstaining from sex for a period of between 2 days to 5 days without sex. It can be produced at the clinic or at home (as long as it arrives within one to two hours of production). (See section on Male Infertility).
Other Fertility Tests and Treatments
If pregnancy does not occur after initial tests, more specialised tests may be useful to further evaluate the uterine cavity and fallopian tubes.
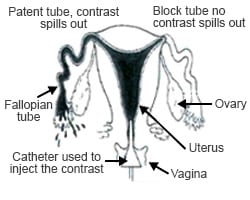

Hysterosalpingogram
This is a radiologic procedure to examine the shape of the uterine cavity and the patency of the fallopian tubes. Women undergoing this test have to lie down and have a speculum inserted into the vagina. A small catheter tube is inserted through the cervix and into the uterine cavity. Radio-opaque contract (liquid) is injected into the uterus. The radiologist can observe the movements of this fluid into uterus and the fallopian tubes and take x-rays to document the results.
As the contrast enters the uterus, the internal contour of the uterus is outlined. Abnormalities inside the uterus cavity may be detected by observing the contrast fluid movement. When there is an abnormality such as a uterine polyp or submucous fibroid, the contrast fluid will move around the polyp or fibroid resulting in a disruption in the outline of the uterine cavity.
As the contrast fills the uterus, it will then enter the fallopian tubes, fill the tubes and spill out of their ends if the tubes are patent (not blocked).
Occasionally, a woman’s fallopian tubes may go into spasm (due to pain or coldness of the contrast) and the flow of contrast stops and does not enter the fallopian tubes. This is not true blockage and further testing by other methods such as laparoscopy may be needed before your doctor can ascertain the patency of the fallopian tubes.
The HSG procedure is not designed to evaluate the ovaries or to diagnose endometriosis, nor can it identify fibroids in the outer wall of the uterus.
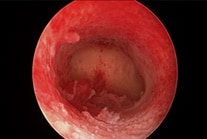

(Left) Hysteroscopy: Normal uterus cavity
(Right) Hysteroscopy: Submucous fibroid bulging into the uterus cavity
Hysteroscopy under mild anaesthesia
Hysteroscopy is a procedure when a small scope is inserted into the uterus via the cervix. The scope is attached to a camera which allows the gynae / fertility specialist to examine the cavity of the uterus and perform minor surgery if required.
Diagnostic Hysteroscopy allows direct visualization of the uterine cavity to confirm the suspected abnormality seen on ultrasound scan or HSG. Therapeutic Hysteroscopy is when minor surgery is performed through this small scope to remove or correct the abnormality found e.g. removal of polyps and small fibroids.
Diagnostic laparoscopy under general anaesthesia
Diagnostic laparoscopy is a surgical procedure where a scope is inserted into the abdominal cavity via a small incision at the umbilicus to assess the internal organs.
The abdominal cavity is distended by introducing CO2 gas inside. In this way the various abdominal & pelvic organs can be seen via the scope with an attached camera. The uterus cavity and fallopian tube can be flushed with blue dye to check for patency of fallopian tubes.
Laparoscopic surgery to correct abnormalities (e.g. scars / adhesions) or remove tumour (e.g. fibroids and cysts) can be done by introducing laparoscopic surgical instruments through an additional 1 to 3 small openings in the abdomen.
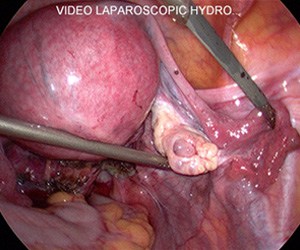

Laparoscopy: showing dye flowing out the fallopian tube
Make An Appointment
Make an appointment online or contact the fertility clinic to consult a fertility specialist. Under Specialist Appointment Details, select "Assisted Reproductive Medicine" or "Obstetrics, Gynaecology & Fertility".
Make an enquiry. We will get back to you within 2 working days. You can reach us at 6311 1250.